Almost 50% of Hospitalized with COVID-19 Had Mild or Asymptomatic Cases
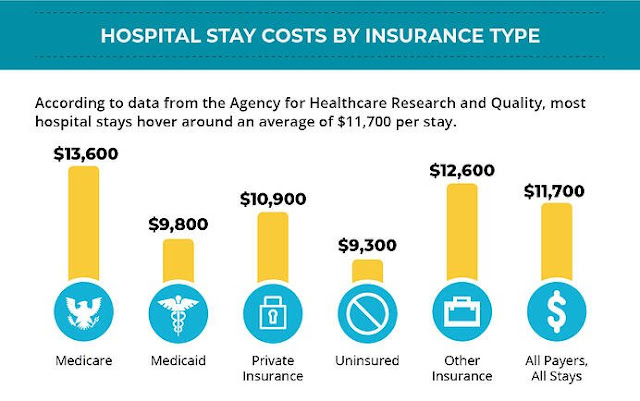
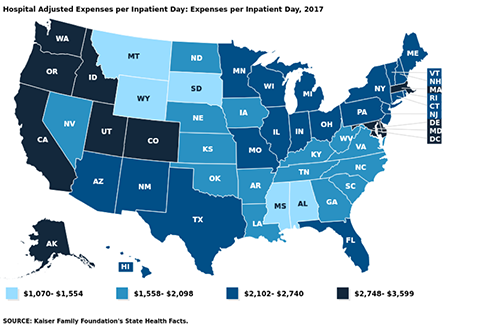
US hospitals typically spend $2,424/day to provide inpatient care. Are hospitalizations another federal money grab?
A new study suggests that almost half of those hospitalized with COVID-19 have mild or asymptomatic cases.
Researchers from Harvard Medical School, Tufts Medical Center, and the Veterans Affairs Healthcare System took on the task of trying to figure out how serious Covid cases were in those hospitalized, and how many people counted as Covid hospitalizations were actually in the hospital for Covid, versus getting a Covid test after being admitted for something else.
The study "analyzed the electronic records for nearly 50,000 COVID hospital admissions at the more than 100 VA hospitals across the country," The Atlantic wrote. It "checked to see whether each patient required supplemental oxygen or had a blood oxygen level below 94 percent" in order to try and determine if cases met the NIH's threshold for "severe COVID".
What the study found was that from March 2020 to January 2021, 36% of Covid cases in the hospital were mild or asymptomatic. From January 2021 to June 2021, during the Delta variant's spread, that number rose all the way to 48%. For vaccinated hospital patients, the number rose to a stunning 57%.
At least 12,000 Americans have already died from COVID-19 this month, as the country inches through its latest surge in cases. But another worrying statistic is often cited to depict the dangers of this moment: The number of patients hospitalized with COVID-19 in the United States right now is as high as it has been since the beginning of February. It’s even worse in certain places: Some states, including Arkansas and Oregon, recently saw their COVID hospitalizations rise to higher levels than at any prior stage of the pandemic. But how much do those latter figures really tell us?
From the start, COVID hospitalizations have served as a vital metric for tracking the risks posed by the disease. Last winter, this magazine described it as “the most reliable pandemic number,” while Vox quoted the cardiologist Eric Topol as saying that it’s “the best indicator of where we are.” On the one hand, death counts offer finality, but they’re a lagging signal and don’t account for people who suffered from significant illness but survived. Case counts, on the other hand, depending on which and how many people happen to get tested. Presumably, hospitalization numbers provide a more stable and reliable gauge of the pandemic’s true toll, in terms of severe disease. But a new, nationwide study of hospitalization records, released as a preprint today (and not yet formally peer-reviewed), suggests that the meaning of this gauge can easily be misinterpreted—and that it has been shifting over time.
If you want to make sense of the number of COVID hospitalizations at any given time, you need to know how sick each patient actually is. Until now, that’s been almost impossible to suss out. The federal government requires hospitals to report every patient who tests positive for COVID, yet the overall tallies of COVID hospitalizations, made available on various state and federal dashboards and widely reported on by the media, do not differentiate based on the severity of illness. Some patients need extensive medical intervention, such as getting intubated. Others require supplemental oxygen or administration of the steroid dexamethasone. But there are many COVID patients in the hospital with fairly mild symptoms, too, who have been admitted for further observation on account of their comorbidities, or because they reported feeling short of breath. Another portion of the patients in this tally are in the hospital for something unrelated to COVID, and discovered that they were infected only because they were tested upon admission. How many patients fall into each category has been a topic of much speculation. In August, researchers from Harvard Medical School, Tufts Medical Center, and the Veterans Affairs Healthcare System decided to find out.
Researchers have tried to get at similar questions before. For two separate studies published in May, doctors in California read through several hundred charts of pediatric patients, one by one, to figure out why, exactly, each COVID-positive child had been admitted to the hospital. Did they need treatment for COVID, or was there some other reason for admission, like cancer treatment or a psychiatric episode, and the COVID diagnosis was merely incidental? According to the researchers, 40 to 45 percent of the hospitalizations that they examined were for patients in the latter group.
The authors of the paper out this week took a different tack to answer a similar question, this time for adults. Instead of meticulously looking at why a few hundred patients were admitted to a pair of hospitals, they analyzed the electronic records for nearly 50,000 COVID hospital admissions at the more than 100 VA hospitals across the country. Then they checked to see whether each patient required supplemental oxygen or had a blood oxygen level below 94 percent. (The latter criterion is based on the National Institutes of Health definition of “severe COVID.”) If either of these conditions was met, the authors classified that patient as having moderate to severe disease; otherwise, the case was considered mild or asymptomatic.
The study found that from March 2020 through early January 2021—before vaccination was widespread, and before the Delta variant had arrived—the proportion of patients with mild or asymptomatic disease was 36 percent. From mid-January through the end of June 2021, however, that number rose to 48 percent. In other words, the study suggests that roughly half of all the hospitalized patients showing up on COVID-data dashboards in 2021 may have been admitted for another reason entirely, or had only a mild presentation of the disease.
This increase was even bigger for vaccinated hospital patients, of whom 57 percent had mild or asymptomatic disease. But unvaccinated patients have also been showing up with less severe symptoms, on average, than earlier in the pandemic: The study found that 45 percent of their cases were mild or asymptomatic since January 21. According to Shira Doron, an infectious-disease physician and hospital epidemiologist at Tufts Medical Center, in Boston, and one of the study’s co-authors, the latter finding may be explained by the fact that unvaccinated patients in the vaccine era tend to be a younger cohort who are less vulnerable to COVID and may be more likely to have been infected in the past.
Among the limitations of the study is that patients in the VA system are not representative of the U.S. population as a whole, as they include few women and no children. (Still, the new findings echo those from the two pediatric-admissions studies.) Also, like many medical centers, the VA has the policy to test every inpatient for COVID, but this is not a universal practice. Lastly, most of the data—even from the patients admitted in 2021—derived from the phase of the pandemic before Delta became widespread, and it’s possible that the ratios have changed in recent months. The study did run through June 30, however, when the Delta wave was about to break, and it did not find that the proportion of patients with moderate to severe respiratory distress was trending upward at the end of the observation period.
The idea behind the study and what it investigates is important, says Graham Snyder, the medical director of infection prevention and hospital epidemiology at the University of Pittsburgh Medical Center, though he told me that it would benefit from a little more detail and nuance beyond oxygenation status. But Daniel Griffin, an infectious disease specialist at Columbia University, told me that using other metrics for the severity of illness, such as intensive-care admissions, presents different limitations. For one thing, different hospitals use different criteria for admitting patients to the ICU.
One of the important implications of the study, these experts say, is that the introduction of vaccines strongly correlates with a greater share of COVID hospital patients having mild or asymptomatic disease. “It’s underreported how well the vaccine makes your life better, how much less sick you are likely to be, and less sick even if hospitalized,” Snyder said. “That’s the gem in this study.”
“People ask me, ‘Why am I getting vaccinated if I just end up in the hospital anyway?’” Griffin said. “But I say, ‘You’ll end up leaving the hospital.’” He explained that some COVID patients are in for “soft” hospitalizations, where they need only minimal treatment and leave relatively quickly; others may be on the antiviral drug remdesivir for five days, or with a tube down their throat. One of the values of this study, he said, is that it helps the public understand this distinction—and the fact that not all COVID hospitalizations are the same.
But the study also demonstrates that hospitalization rates for COVID, as cited by journalists and policymakers, can be misleading, if not considered carefully. Clearly many patients right now are seriously ill. We also know that overcrowding of hospitals by COVID patients with even mild illness can have negative implications for patients in need of other care. At the same time, this study suggests that COVID hospitalization tallies can’t be taken as a simple measure of the prevalence of severe or even moderate disease, because they might inflate the true numbers by a factor of two. “As we look to shift from cases to hospitalizations as a metric to drive policy and assess the level of risk to a community or state or country,” Doron told me, referring to decisions about school closures, business restrictions, mask requirements, and so on, “we should refine the definition of hospitalization. Those patients who are there with rather than from COVID don’t belong in the metric.”
Among the limitations of the study is that patients in the VA system are not representative of the U.S. population as a whole, as they include few women and no children. (Still, the new findings echo those from the two pediatric-admissions studies.) Also, like many medical centers, the VA has a policy to test every inpatient for COVID, but this is not a universal practice. Lastly, most of the data—even from the patients admitted in 2021—derive from the phase of the pandemic before Delta became widespread, and it’s possible that the ratios have changed in recent months. The study did run through June 30, however, when the Delta wave was about to break, and it did not find that the proportion of patients with moderate to severe respiratory distress was trending upward at the end of the observation period.
Popular Posts (All Time)
-
Table of Contents Introduction: Stress, Smoking, and Health The Normotim Effect: A New Hope in Stress Management Lithium Ascorbate:...
-
The coronavirus disease (COVID-19) pandemic has been linked to mental health issues related to disease-induced morbidity and mortality and p...
-
A group of virologists in February 2020 published a letter in The Lancet stating they “overwhelmingly conclude that this coronavirus origina...
-
SAMPLE LETTER BELOW 🚨🚨🚨 The secret is NOT to refuse the Jabb.... From a lawyer: If you are being forced to Vax in order to keep your job,...
-
Former Hunter Biden business partner Tony Bobulinski has confirmed that an email published in the New York Post's bombshell exposé is i...
-
The time is now. As most readers of this substack are now well aware, this is not just about COVID. The Constitution hangs in the balance. P...
-
Klaus Schwab's World Economic Forum Government & WHO Lies Tucker & Malone Discuss The World Economic Forum & It's Young ...
-
Comment to ACIP meeting of August 30, 2021 submitted by Steve Kirsch - Executive Director of the COVID-19 Early Treatment Fund stk@treatearl...
-
Crimes Against Humanity - The PCR Test Fraud and COVID-19 will be the Case of the Century Reiner Fuellmich - Update on Court Case & P...
-
2 Sources for this story below . . . Justin Bieber reveals he has Ramsay Hunt syndrome Twitter suspended the VaccineTruth2 account Want to ...